How SSc can affect the GI tract
The mouth
Thinning of the upper lip and reduction in mouth opening may affect what a someone is able to eat comfortably. Oral dryness may also affect dental health. Telangiectasia means red vascular mucosal lesions in the mouth that may occasionally bleed.
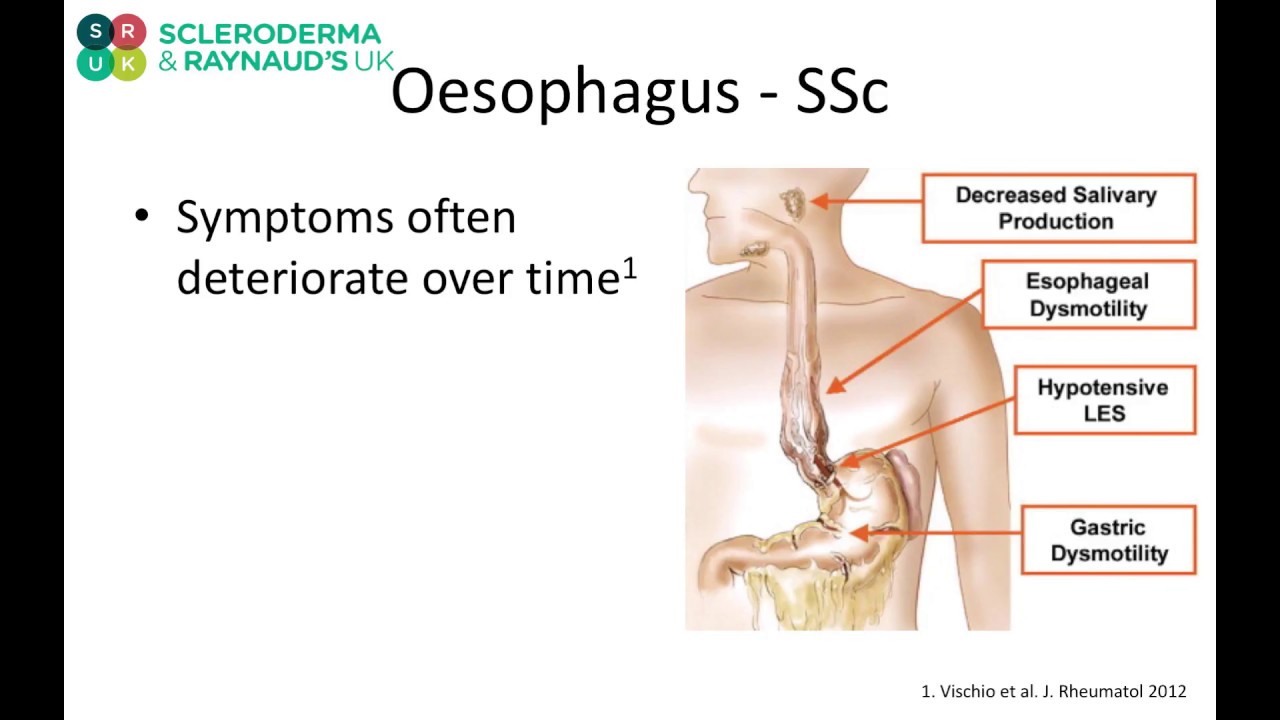
The oesophagus
The oesophagus (gullet) runs from the mouth to the stomach. It is affected in most patients with SSc (80-90%), although this will not always cause any symptoms.
Gastro-oesophageal reflux occurs when acid from the stomach slips back into the oesophagus, which can lead to other complications such as oesophagitis, strictures (narrowing due to fibrosis) and Barrett’s oesophagitis (mucosal changes that require surveillance as there is a risk of developing malignant changes). Typical symptoms include difficulty swallowing, heartburn and water brash/reflux. Severe reflux can also result in acid spilling over into the lungs, that can aggravate any lung involvement.
The stomach
The stomach is less commonly involved in SSc. The two main features are:
- Vascular lesions (e.g. gastric antral vascular ectasia), which can lead to bleeding (acute and chronic) and anaemia
- Delayed emptying of the stomach with bloating due to dysmotility, that may contribute to reflux
The small and large intestines
The small intestine absorbs nutrients from food that is digested, whereas the main function of the large intestine (the colon) is to reabsorb water and salts that have been secreted by the rest of the gut, as well as the disposal of waste. Both the small and large intestines may be affected in several ways, including reduced movement, reduced absorption (of various minerals/vitamins/iron/fatty acids), and overgrowth of bacteria.
Anorectum
The rectum is designed to hold faeces until the bowels are emptied, maintaining continence with the help of the anal sphincters. If anorectal involvement in scleroderma is not managed effectively, it may lead to rectal prolapse and thinning of the anal sphincter, as well as incontinence.
Diagnosis
Testing is an essential part of the management of SSc, and this can detect signs of GI tract involvement at an early stage. Your doctor may diagnose your GI tract involvement in SSc by asking about your medical history to learn about signs and symptoms, as well as possible risk factors. Relevant tests are described below.
Gastroscopy
A procedure done usually under sedation where a flexible telescope is passed by the mouth down into the stomach. A paediatric scope, which is smaller, may be used to minimise discomfort caused by a smaller opening. It allows direct vision of the oesophagus, stomach and first part of the small intestine. Biopsy (extracting cells) of the mucosal surfaces may be taken to evaluate any changes.
Oesophageal physiology studies
This involves a small tube being passed from the nose to the stomach. The amount of acid reflux can be measured by a 24- hour study, again involving a small tube passed from the nose to the oesophagus.
Barium Swallow
A barium swallow is an examination of the oesophagus and the stomach. This test will be conducted by a radiologist (a doctor who uses x-rays to diagnose and treat illnesses), and a radiographer (a health professional that produces the images used to diagnose and treat illnesses).
The procedure uses a type of X-ray called fluoroscopic imaging to view images in real time. These areas of your body cannot normally be seen on X-ray images, so you will be required to swallow contrast material. This enables your doctors to evaluate the surface changes as the contrast material passes through the oesophagus and stomach. The images are taken as you swallow the liquid and as it passes into your stomach. The radiologist can check the oesophagus and stomach and see how well the liquid moves through them.
Endoscopy
An endoscopy is a procedure where organs inside your body are looked at using an instrument called an endoscope. An endoscope is a long, thin, flexible tube that has a light and camera at one end. Images of the inside of your body are shown on a television screen. This test can also detect and help manage strictures (narrowing of the esophagus).
Oesophageal Manometry
Oesophageal manometry is a test used to measure the pressure and functioning of the muscles of the oesophagus and the sphincter leading to the stomach. This indicates how well the muscles are performing as food and liquids pass from mouth to the stomach
MRI (magnetic resonance imaging) scan
This test uses magnetism to create a detailed image of areas of your body. This scan may be used to assess whether the GI tract is involved in SSc. Sometimes people are injected with a dye (contrast medium) to help make images show up more clearly. The procedure (carried out by a radiographer) is painless, however you may find it a little uncomfortable as you have to lie in a long tube for about 30 minutes. Importantly, you can only have the scan if you do not have any metal within your body (i.e. dental wires or metal plates). With MRI, patients do not have any radiation exposure.
Hydrogen or Lactulose breath test
This requires ingestion of a sugary solution and testing for serial breath samples over several hours. This may be considered in cases of suspected bacterial overgrowth.
Anorectal physiology studies
These are tests that check the function and structure of the anal sphincters and rectum and involve a small probe inserted at the tail end.
Treatment
There are several treatments available for GI tract involvement in SSC, and the best option will always depend on your individual situation.
Types of treatment
You may suffer from poor oral intake and weight loss. Consuming small, but frequent meals, and nutritional and vitamin supplements can help many patients. Sometimes more extreme approaches are needed if you suffer from severe weight loss and malnutrition and are unable to eat adequately by mouth, such as having a small tube passed into the stomach, nasogastric tube (where a tube is inserted through the nose and throat into the stomach), percutaneous endoscopic gastrostomy (PEG; where a flexible feeding tube is placed through the abdominal wall and into the stomach) or intravenous feeding (tube inserted into veins).
Reflux can be treated with anti-reflux medications (proton pump inhibitors and antacids e.g. Gaviscon Advance, Rennies). If you suffer from dysmotility (swallowing difficulties, nausea, vomiting), this can be helped by prokinetic medications, such as domperidone, metoclopramide, and prucalopride.
Gastric antral vascular ectasia (GAVE or bleeding from stomach) can be alleviated with iron supplements (tablets or intravenous formulation) or endoscopic treatment with thermal/radiofrequency methods to stem the bleeding points.
Small bowel bacterial overgrowth can be managed with antibiotics. Either single course or cyclical courses may be required, and this largely depends on frequency and severity of your symptoms. Adjusting your diet can also help to alleviate symptoms of bacterial overgrowth.
Constipation and diarrhoea can be managed symptomatically but judicious use is required as some individuals may experience both constipation and diarrhoea.
Bowel rest may be required on occasion for severe cases of non-mechanical bowel obstruction. This often requires medical evaluation with inpatient admission.
Faecal incontinence is often a challenge, and this requires careful evaluation with your gastroenterologist. Obstetric history with forceps delivery may be relevant in some cases. In some selected cases, nerve stimulation to the anorectal apparatus can be considered. Pelvic floor physiotherapy can also be helpful.
Treatment for your anorectum is tailored to your individual’s symptoms and the abnormalities found. Many different treatments can be used and are often very effective. Practical changes, such as raising the head of the bed, can be very helpful to give immediate relief. You may suffer from diarrhoea and incontinence, treatment for this include loperamide and opiates. More specialised treatments maybe required such as trans-anal irrigation, sacral nerve stimulation, surgery (e.g. rectal prolapse repair).
More information and finding support
SRUK are here to support you and we offer a number of ways to access information and resources, find support and connect with others who may be in a similar situation. Please give us a call on 020 3893 5998 and we will be very happy to help you.
Social media
Our Facebook, Twitter, Instagram and Youtube pages are designed to enable you to interact with others, discuss different issues and share advice. You can also help us to raise awareness of Scleroderma and Raynaud's by sharing web pages using the share buttons.
Join our online community
You can also visit our online community hosted on the Health Unlocked website. This is a friendly space where you can chat with other people who are affected by scleroderma, exchange advice and information and share support.
Ask us a question
If you have a question and you cannot find the answer, please contact us at info@sruk.co.uk and we can forward it to a specialist on your behalf.